Understanding Diabetes
Diabetes is a condition that occurs when blood sugar (glucose) levels are too high. The three most common types are Type 1, Type 2, and gestational diabetes. In Type 1 diabetes, the immune system destroys the pancreatic cells that make insulin, so people must take insulin daily to survive. Type 2 diabetes, the most common form, occurs when the body doesn’t use insulin properly or doesn’t make enough, leading to high blood sugar. Gestational diabetes develops during pregnancy and usually goes away after birth, though it increases the risk of developing Type 2 diabetes later.

136 million Americans have diabetes or prediabetes.
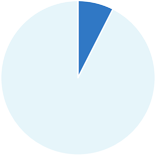
5-10% of people with diabetes have Type 1.
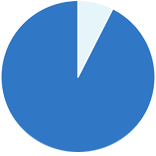
90-95% of people with diabetes have Type 2.
When diabetes is not controlled, patients’ high glucose levels can lead to serious health complications and even death. In fact, diabetes is the eighth-leading cause of death in the United States. According to the CDC, 38 million Americans have diabetes, while 98 million – over one-third of U.S. adults – have prediabetes, and more than 80 percent are unaware of having prediabetes.
How Diabetes Impacts Health
- Over time, diabetes can damage the heart, blood vessels, eyes, kidneys, and nerves.
- Adults with diabetes are two to four times more likely to have a stroke or heart disease due to high blood glucose damaging blood vessels and nerves.
- Nerve damage and poor foot circulation increases the chance of foot ulcers, infection, and amputation. Diabetes accounts for more than 60% of non-traumatic lower-limb amputations.
- Diabetic retinopathy, caused by damage to the retina’s small blood vessels, is a leading cause of adult blindness.
- Chronic kidney disease affects about one in three adults with diabetes, making kidney damage a common complication.
Medtech’s Role in Improving Diabetes Care
Early diagnosis and treatment of diabetes can lead to improvements in the long-term health outcomes of patients. AdvaMed members are developing new technologies that make day to-day life healthier and easier for those living with diabetes and allow patients to manage their diabetes more effectively, improving their care outcomes in the process. These include continuous glucose monitors (CGMs), which automatically track glucose levels day and night, allowing persons with diabetes to see where their glucose values have been, where they are now, and where they are going, compared to the older traditional blood glucose monitors (BGMs).
BGMs are the most common alternative to CGMs, but they only provide point-in-time data
and often miss important high or low blood glucose level episodes. Thanks to advancements
in medical technology, CGMs can fill in important data gaps and even alert the patient in real
time of a high or low glucose episode so they can immediately bring their glucose back into
an optimal range. CGMs generally consist of a sensor/transmitter that is worn on the body to
measure glucose data and a reader or smartphone that allows users to view current and
past glucose readings.

CGMs are often used with insulin pumps, which are small, computerized devices that deliver insulin as needed, including in bolus doses close to mealtime, to control the rise of blood sugar after a meal, mimicking the body’s normal release of insulin.
It is now possible to combine CGMs and insulin pumps into an automated insulin delivery (AID) system, which can also be referred to as a loop or an artificial pancreas. With an AID system, patients can rely on their CGM readings to guide their insulin pump, requiring less user input than when the two technologies are separate.


